Note: Dr. John Hearnsberger of Nashville continued his series of weekly updates on coronavirus Sunday morning, April 26, at First United Methodist Church of Nashville.
HMH continues its lockdown. Last Monday we had our first overflow of patients to the bed space available in the OR, specifically the pre-op/recovery areas. There were enough discharges Tuesday to move all of these patients back to the west wing. Saturday morning the west wing was again at capacity, and any admissions would overflow to the OR. By Saturday afternoon, the east wing again was again open and remains open this morning.
Elective surgical cases can resume tomorrow [Monday] with some rather stringent criteria outlined by the Ark. Department of Health in conjunction with The Ark. Chapter of the American College of Surgeons. The most difficult guideline for us to follow—A negative COVID-19 test within 48 hours of the scheduled procedure. This is difficult because these tests are sent to a reference lab and the turnaround time varies from 24 hours up to 4 days. More and more tests are being done which burdens the labs and increases the turnaround time. Small rural hospitals and critical access hospitals, such as HMH, are exempt from these guidelines. However, HMH Surgery Dept. will make every effort possible to follow these guidelines. We will probably exceed the 48 hr. testing guideline in most cases, but we will test all patients for elective surgeries.
Here are the latest Ark. COVID-19 statistics from this morning–
1. Total cases—2909.
2. Total deaths—Democrat-Gazette 48. Ark. Dept. Health 49.
3. Recoveries—985.
4. Positive tests—2909.
5. Total tests done—38,163.
6. Negative tests—35,254.
7. 71/75 counties affected, and 13 cases are in Howard County. If the Health Dept. web site is correct, we have no new cases this week.
Television news, which is inundated with COVID-19 stories, along with newspapers, have an increasing number of stories about reopening the economy and possible resurgence of COVID-19 infections. There was a news story this week about a resurgence of infections in northern China along the Russian border.
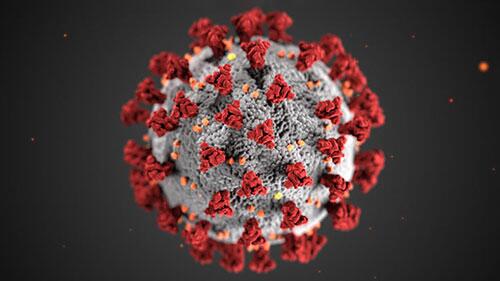
Let’s take a few minutes and look again at the Spanish Flu, an H1N1 virus, and draw possible or potential comparisons to this current pandemic, SARS-CoV-2 or COVID-19 due to the coronavirus. First and foremost, let me emphatically state that our overall medical knowledge, our understanding of infectious disease transmission and treatment, and our many life saving medical interventions are light years ahead of what the medical community knew or practiced in 1918. There is no comparison of then to now in medical knowledge. But can we compare, or draw parallels, the two pandemics?
The Spanish Flu first appeared in March 1918 and had all the hallmarks of seasonal flu. One of the first registered cases was in Albert Gitchell, a military cook stationed in Kansas, and the virus spread quickly through the 54,000 troups stationed at Camp Funston. By the end of March, 1,000 troops were infected and 34 died. As troops moved en masse to the war in Europe, they carried the virus with them. Throughout April and May the virus spread rapidly throughout England, France, Spain, and Italy. Supposedly 3/4 of the British military and 1/2 of the French military were infected. Luckily, the first wave of influenza was not that deadly, and symptoms were fever and malaise, similar to the seasonal flu.
Spain was neutral during WW1. The press in other countries were not allowed to print negative stories that could harm the war effort. Thus, the Spanish journalists were the only ones reporting on this widespread illness, which became known as the Spanish Flu.
Flu cases dropped off through the summer of 1918. Somewhere in Europe during the summer, a mutated strain of the virus emerged, was especially virulent, and able to kill a healthy young man in 24 hours of developing signs of the infection .
In August 1918, military ships departed England carrying troops infected with this virus. As these ships arrived in ports in Europe, the US, and West Africa, the second, more deadlier wave of the pandemic began. This massive troop movement around the world was a major factor in the global spread of the virus.
From September through November of 1918 the cases and deaths skyrocketed. What is termed a “W” curve was exhibited. Unlike normal seasonal flu that kills primarily the young and the old, there was a mortality spike in healthy 25-35 year olds in the prime of their life.
This H1N1 pandemic in 1918 infected 500,000,000 world wide and killed 50,000,000. 675,000 died in the US. There is no doubt that close quarters, poor sanitation, and little understanding of the spread of infectious pathogens, plus lack of knowledge of viruses, fueled this fire.
The H1N1 epidemic of 2009-10 was a variant of the Spanish Flu virus. We had no vaccine at the outbreak, and it killed 12,469 in the US and over 152,000 world wide. Since the initial outbreak of COVID-19 in China in December 2019, there are 2,897,645 cases worldwide with 202,880 deaths. 939,053 cases in the US with 53,789 deaths, according to the morning paper.
So what do these two pandemics have in common?
1. A highly contagious, deadly virus.
2. Rapid transports of large groups of people around the world. In WW1 it was large groups of troups transported by ships for the war effort in Europe. Today we have planes and ships traversing the globe on business and pleasure each day.
3. We have a virus that mutates. The H1N1 mutated into a more virulent strain in the summer of 1918 that was lethal in 24 hours. Most agree the coronavirus mutates. That could explain a variance in symptoms and in the clinical course of those infected. Mutation changes the makeup or then genetic code. Vaccines or medicines developed to prevent or treat a certain viral infection may be rendered ineffective against a mutated virus. This is a significant part of the problem in developing a vaccine for the HIV/AIDS virus. We all are aware that bacteria develop antibiotic resistance.
4. No effective prevention or treatment to date, although many clinical trials are underway.
The question is, “Will we have a resurgence of COVID-19 this fall.” Given the above 5 correlations, the short answer, in my opinion, is, “Yes.” The virus is not going anywhere and will still be with us.
If we are unable to develop a vaccine to prevent infections, nor a drug to treat those infections, we will see a resurgence of this viral illness, probably coinciding with seasonal flu. Furthermore, we do not yet know if development of antibodies to coronavirus from having had the infection, will protect one from becoming re-infected. But because of modern medicine, knowledge of viral infections, and the best medical care in the world, the impact will be far less.
How long do we shut down our economy? When do we restart? We have multiple millions unemployed, and record numbers each week applying for unemployment. How long? At what cost? A lot of important questions must be answered.
We must, as a nation, analyze all data carefully, logically, and scientifically to prepare for a resurgence of the coronavirus, plus prepare for future epidemics or pandemics. One thing we, the people, must not do is allow partisan politics to interfere.
Thanks to all who feed us, keep us safe, and healthy.
“Now go out into the world and treat everyone you meet exactly like you want them to treat you.” Masterson.